As CMS raises expectations for Plan Year (PY) 2026, network adequacy has become a defining element of Qualified Health Plan (QHP) certification. The focus has shifted toward earlier validation, tighter alignment across data sources, and defensible provider access at scale.
For health payers, this shift reinforces a broader reality. Network Adequacy (NA) is no longer a downstream compliance task; it is a strategic capability that influences certification confidence, operational planning, and market stability.
This article outlines how CMS expectations are evolving for PY2026. It examines why traditional QHP preparation approaches cause friction. It also explains how HiLabs® NetworkIQ enables payer operations teams to manage network adequacy with greater clarity, consistency, and control.
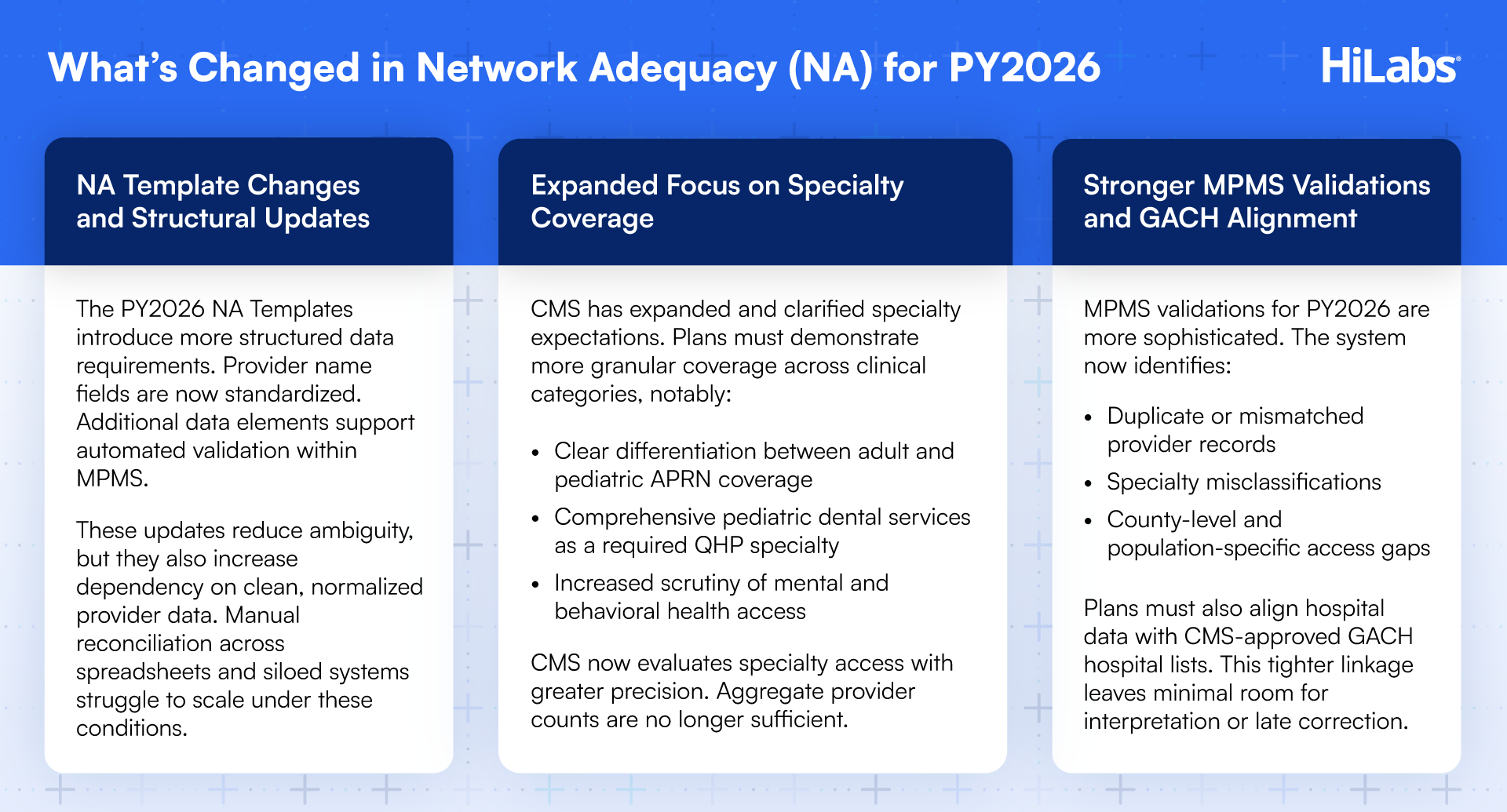
What CMS Expects for PY2026
For PY2026, CMS is elevating expectations around the quality and defensibility of network adequacy submissions. Reviews are increasingly centered on provider access realism, specialty coverage accuracy, and consistency across submitted data sets.
CMS expects network adequacy data to align with real-world provider access conditions. Provider records should be consistent across specialties, locations, and service areas. NA Templates must withstand automated validation and manual review.
Key focus of CMS requirements for PY2026 includes:
Accurate time-and-distance calculations at the county level
Clear specialty alignment, including pediatric, dental, and behavioral health
Consistency between provider data and CMS-approved reference sources
Reduced reliance on post-submission corrections and manual justification
Considering these changes, plans that surface adequacy gaps sooner will retain greater flexibility. Late discovery limits remediation options and increases operational strain during certification review.
Why PY2026 QHP Filing Is a High-Risk Moment for Health Plans
QHP filing plays a pivotal role in confirming readiness for ACA Marketplace participation. Certification outcomes influence enrolment planning, market presence, and financial forecasting. As a result, QHP filing supports revenue stability and operational continuity.
For PY2026, CMS validation changes increase the importance of early accuracy and alignment. Network adequacy submissions are reviewed earlier in the cycle; opportunities for late-stage adjustments are more limited.
Health plans face several elevated risks:
Earlier detection of provider data inconsistencies
Reduced flexibility to remediate adequacy gaps after submission
Greater likelihood of extended certification review cycles
For multi-state plans or organizations pursuing growth, these pressures scale quickly. Network adequacy readiness now requires executive oversight well ahead of submission timelines.
Where Traditional QHP Preparation Falls Short
Many health plans still rely on legacy workflows to prepare for QHP filing. These approaches were not designed for the pace, scale, or scrutiny of PY2026 requirements.
Common limitations include:
Fragmented provider data across claims, credentialing, and directories
Manual NA Template reconciliation
Limited specialty-level visibility
Inconsistent tracking of telehealth access
Reactive mitigation under compressed timelines
These constraints introduce uncertainty. Certification timelines become harder to predict, and strategic planning becomes more cautious.
How HiLabs® NetworkIQ Supports QHP Filing Readiness for PY2026
NetworkIQ by HiLabs® is purpose-built to address modern network adequacy challenges. It replaces brittle, manual workflows with automation, analytics, and decision intelligence.
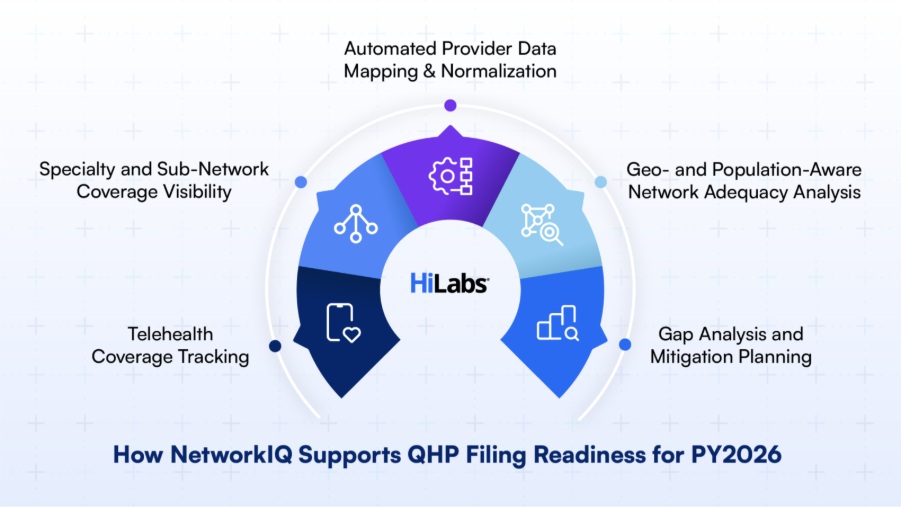
Automated Provider Data Mapping and Normalization
NetworkIQ ingests provider data from claims systems, credentialing platforms, directories, and NPPES. It normalizes this data into a CMS-ready structure, aligning it with the updated NA Template requirements.
This improves consistency, not only by reducing formatting errors but also by lowering the risk of MPMS validation failures.
Geo- and Population-Aware Adequacy Analysis
NetworkIQ evaluates access using county-level time-and-distance standards. It applies these rules by specialty and relevant population groups.
Plans gain earlier visibility into readiness across markets. Adequacy gaps surface before Marketplace submission, while remediation options remain available.
Specialty and Sub-Network Coverage Visibility
NetworkIQ tracks and verifies coverage across:
Primary care
Adult and pediatric specialties
Pediatric dentistry
Mental and behavioral health
This unmatched visibility supports the expanded specialty requirements emphasized in PY2026.
Telehealth Coverage Tracking
NetworkIQ tags and identifies providers offering telehealth services and incorporates this data into adequacy analysis. This supports access strategies in rural and underserved areas, where traditional provider coverage may be limited.
Gap Analysis and Mitigation Planning
NetworkIQ enables plans to:
Model provider additions and recruitment strategies
Test contracting strategies
Validate adequacy scenarios
Operations team using NetworkIQ can complete gap analysis and mitigation all well ahead of the CMS certification window.
Why NetworkIQ for QHP Filing
NetworkIQ is not a generic analytics solution. It is designed specifically for healthcare network intelligence and adequacy management.
Plans adopt NetworkIQ because it:
Continuously checks CMS and state adequacy rules
Delivers over 95% accuracy in adequacy gap closure simulations
Reduces review cycles by more than 70%
Supports compliance, competitiveness, and cost-of-care optimization
By aligning these priorities in one platform, NetworkIQ supports the full complexity of modern QHP filing.
Is NetworkIQ for You?
QHP filing outcomes impact executive owners across the enterprise. NetworkIQ supports all teams accountable for successful filings, including:
ACA Marketplace health plans
Network strategy and operations leaders
Compliance and regulatory executives
Provider data and analytics teams
Whether operating in one state or across multiple markets, PY2026 demands greater precision at scale, with limited tolerance for late-stage corrections.
Get Ready for PY2026 QHP Filing
PY2026 is not the year to rely on spreadsheets or last-minute fixes. Health plans that prepare early, validate continuously, and automate network adequacy analysis approach certification with confidence.
Learn more about how NetworkIQ can help you get ready.
Additional Resources:
CMS QHP Certification & Network Adequacy: https://www.qhpcertification.cms.gov
CMS Final Letter to Issuers (PY2026): https://www.cms.gov
