
MCheck VBC
Ensuring payment and data integrity in Value-Based Care
AI-powered automation for member attribution, contracts configuration, and payment integrity—driving efficiency and trust in your VBC programs.
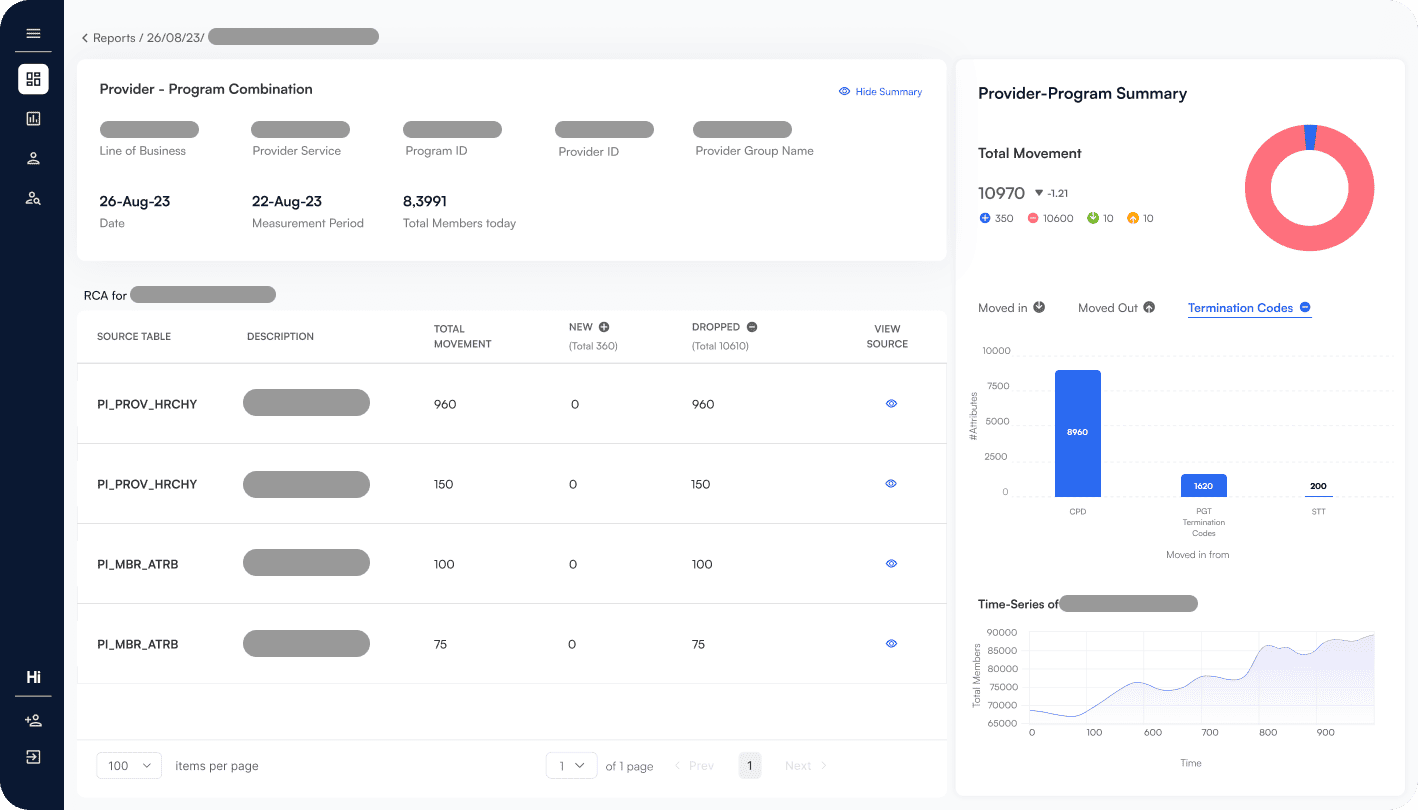
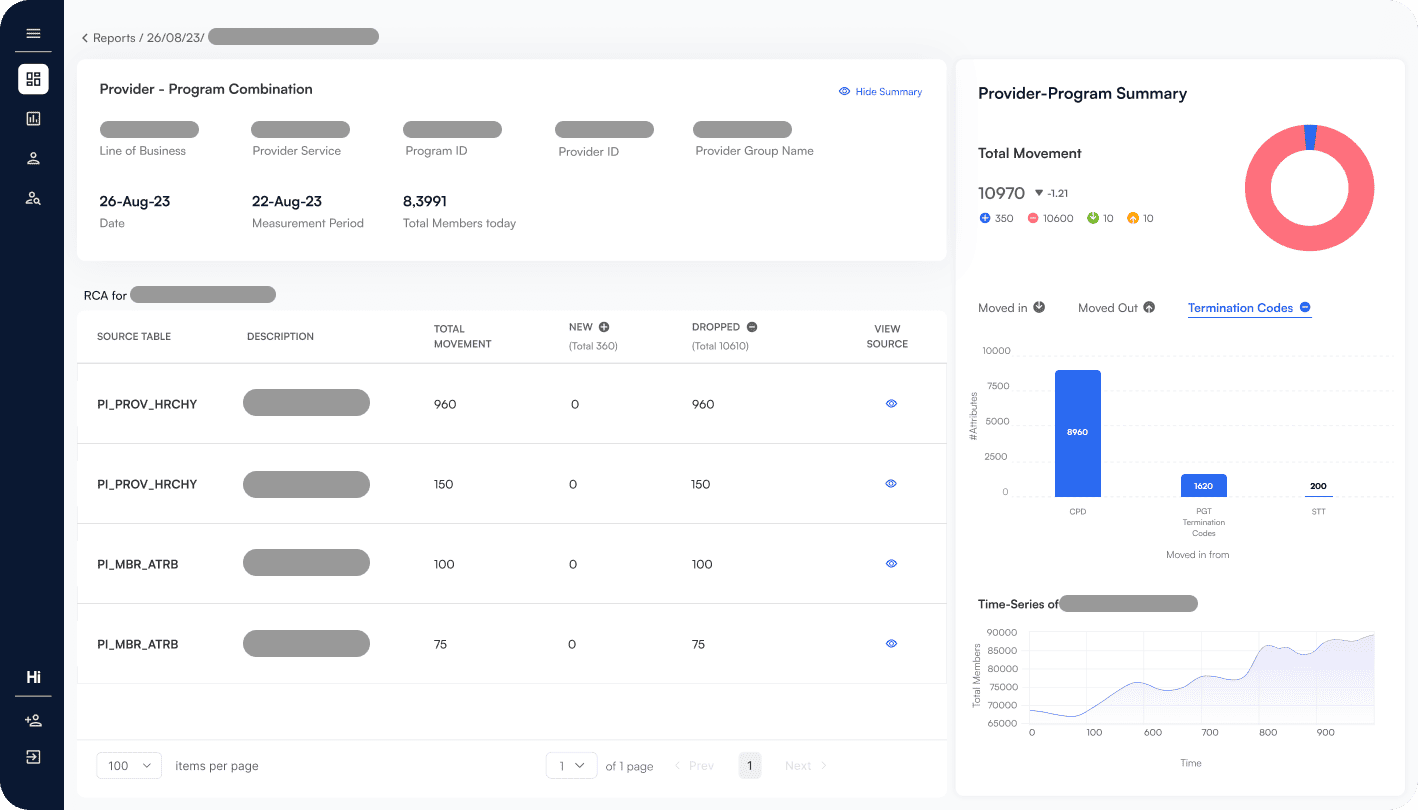
AI-powered anomaly detection and intelligent insights driving financial accuracy and building provider trust
20978+
Anomalies identified across member attributions and provider payments
5978+
Provider groups analyzed daily for anomalous attributions
0M+
Financial transactions audited monthly for anomalous payments
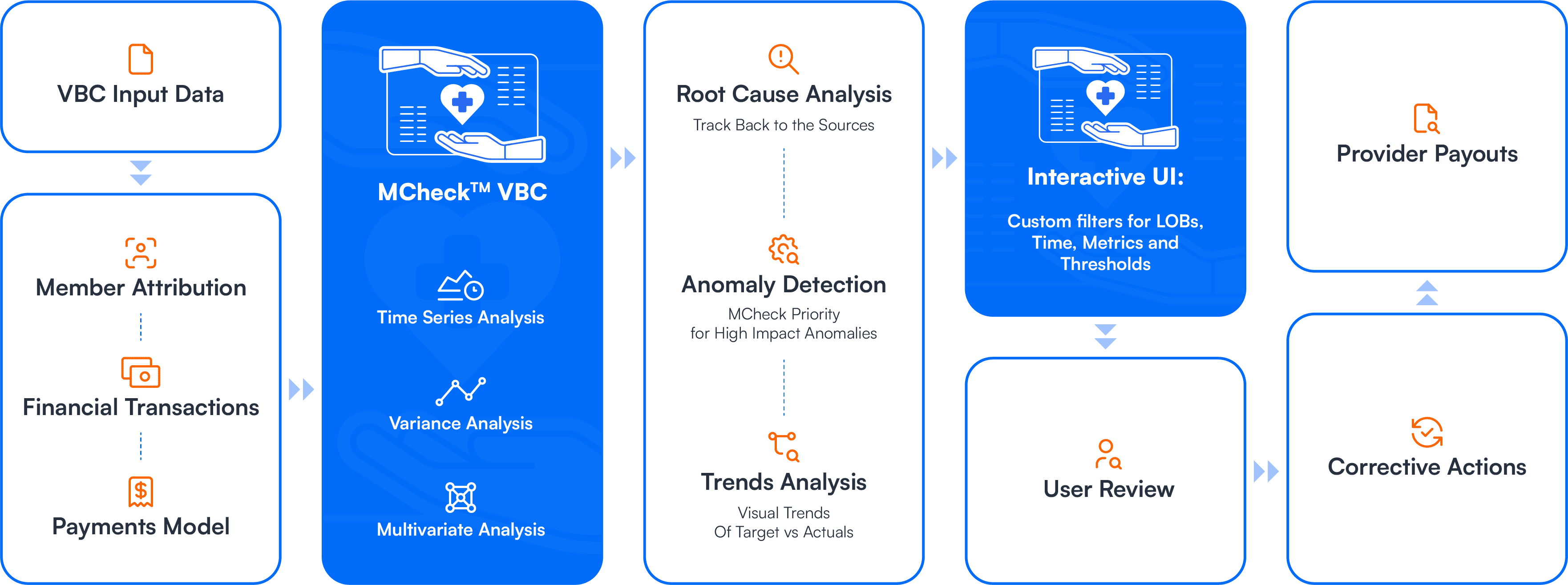
From Plan-Specific Inputs to Trusted Provider Outputs—in Real Time
Legacy Process Challenges vs. HiLabs AI-Powered VBC Solution
Attribution & Program Accuracy
Anomaly Detection & Resolution
Operational Cost & Efficiency
Provider Experience & Flexibility
Attribution & Program Accuracy
Anomaly Detection & Resolution
Operational Cost & Efficiency
Provider Experience & Flexibility
Traditional
Manual attribution reviews lead to low coverage and incomplete findings
HiLabs
Real-time attribution validation analyzing all provider groups across all programs leading to full coverage of anomalies along with RCAs
Why Leading Payers Choose HiLabs AI-Driven Value-Based Care Solution
Comprehensive, AI-powered solution designed to detect, resolve, and prevent value-based care payment issues at scale

Intelligence Engine for Risk & Reconciliation
Proactive Anomaly Intelligence
AI-first detection of high-impact data and payment anomalies—prioritized by HiLabs proprietary scoring system to focus on the greatest operational and financial risk
Multi-Model Payment Reconciliation
Seamlessly supports PMPM, capitation, care coordination, and shared savings models with automated attribution and contract-aligned reconciliation logic
Attribution & Insights for VBC Acceleration
Attribution-Driven VBC Adoption
Enhances member attribution visibility and aligns high-potential providers to the right programs, boosting engagement and accelerating VBC adoption
Smart Views & AI-Powered Tracking
Track financial changes, variances, and trends with intelligent filters and dashboards tailored to business lines, rules, and regions for faster, data-driven decisions
Real Impact, Real Outcomes—What Success Looks Like with HiLabs VBC
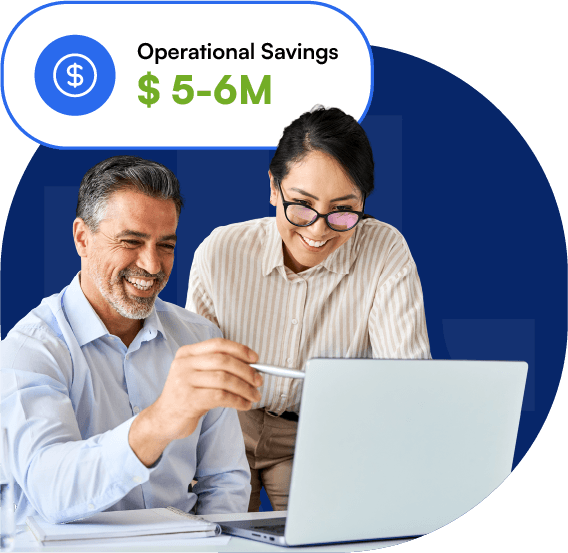
$5–6M in Operational Savings
HiLabs AI-driven anomaly detection and root cause analysis have significantly reduced manual effort, streamlined workflows and unlocked millions in cost savings
Significant Drop in Provider Abrasion
Accurate payments and real-time member attribution have driven transparency and trust, leading to meanignful reductions in provider disputes
Increase in VBC Program Adoption
With clearer insights and targeted engagement, provider participation in VBC programs has increased significantly across supported markets
MCheck Platform
Explore Other MCheck Solutions




