Provider data management is the foundation of accurate networks, compliant directories, and trusted member experiences. Yet for many health plans, provider data remains fragmented, outdated, and difficult to govern. Poor provider data management leads to directory inaccuracies, regulatory risk, and provider abrasion—the day-to-day friction we all experience in healthcare.
In this guide, we break down what provider data management really means for health plans, why provider data accuracy is now a business imperative, how AI platforms, like HiLabs, help health plans scale their accuracy and compliance, and what this shift means for the payer team across network, compliance, and provider operations.
What Is Provider Data Management and Why It Matters
Provider Data Management (PDM) refers to the end-to-end, ongoing process of collection, validation, maintenance, and distribution of accurate healthcare provider data across payer systems. In practice, this includes the data itself, and the workflows required to keep it consistent across systems.
Provider data typically includes a provider’s contact information (name, practice locations, phone numbers), working hours, specialty, network participation, and whether they are accepting new patients.
This is why maintaining accuracy in provider data is critical. Even small discrepancies—such as a location mismatch or incorrect participation status—flow downstream and hinder members’ accessibility to care.
It can also create downstream operational rework when payer teams must resolve the same discrepancies across credentialing, claims, and directory systems. This impacts operational efficiency, which in turn affects both network adequacy compliance and provider and member trust.
In the US, CMS requires health plans to verify and update their provider information at least every 90 days to remain compliant, making scalable provider data management solutions essential for compliance. (See: CMS Provider Directory Rules)
Why Provider Data Accuracy Matters Now More Than Ever
Poor provider data accuracy is no longer just an operational issue; it’s a regulatory and financial risk. When provider data is inaccurate, members are the first to feel the pain. Care is delayed or even disregarded. Member complaints go up, increasing call center volume and the cost of member operations. Regulatory penalties (such as those under No Surprises Act) become a serious risk. Ultimately, bad data erodes the health plan’s brand trust and leads to member churn.
How big is the provider data problem? A 2023 study cited in the Journal of the American Medical Association (JAMA) shows that over 80% of provider directories contain inaccuracies, highlighting the full extent of the problem at hand. (See full research by HiLabs in collaboration with CU School of Medicine)
Key Challenges in Provider Data Management Today
Fragmented Data Sources
Provider data is spread across credentialing systems, claims platforms, CRM tools, and external sources like CAQH, often without synchronization. This fragmentation creates conflicting records and delays updates as different systems may store different “versions” of the same provider record, with inconsistent refresh cycles and ownership.
Low Provider Data Accuracy
Manual updates, infrequent attestations, and inconsistent data formats lead to stale and unreliable provider records across systems. Accuracy gaps persist because updates are often event-driven (credentialing, contracting, claims changes) while directories and network reporting require continuous validation.
Ghost Providers
Ghost providers—providers listed as “in-network” but unavailable—are a major contributor to directory inaccuracies. The No Surprises Act has significantly increased scrutiny around ghost provider cleanup as inaccurate listings can directly affect member access and the plan’s ability to demonstrate directory integrity. (See: CMS NSA Enforcement)
Siloed Provider Data Workflows
Disconnected teams across network operations, compliance, IT, and provider relations slow down corrections and make accountability unclear. In practice, siloed intake and remediation workflows mean the same discrepancy can be worked multiple times—or corrected in one system and missed in another.
Common Limitations of Traditional Provider Data Management Approaches
While there exists a variety of approaches including manual data processing, point solutions and legacy systems, they are all subject to various limitations, such as:
Manual Validation Cannot Scale
Spreadsheet-based audits and random sampling cannot keep pace with real-time provider changes across large networks. Historically, plans have addressed this by increasing staff or extending audit cycles, which may help solve the problem in the short term but does not fix the underlying constraint: validation remains periodic, labor-intensive, and disconnected from how frequently provider data actually changes.
Rule-Based Systems Miss Context
Traditional rules engines struggle with nuance, such as identifying subtle indicators of ghost providers or conflicting location data. These systems evaluate provider attributes in isolation—often as static fields or one-time checks—failing to account for how provider data changes across systems, time, and real-world activity. And so, they fail to identify patterns that only become visible when provider attributes, utilization signals, and network participation data are evaluated together.
Retrospective Provider Data Corrections
Most legacy systems detect errors only after member complaints, access issues, or regulatory findings. By the time these issues surface, inaccurate records may have already propagated across directories, reporting workflows, and downstream operational systems, making remediation slower and more disruptive.
How AI Improves Provider Data Quality
AI-driven provider data management transforms how health plans maintain accuracy by shifting from reactive cleanup to proactive intelligence. Rather than relying on periodic audits alone, AI can support continuous validation and help teams prioritize remediation where it matters most.
For example, AI can help health plans continuously monitor provider signals across systems, detect inconsistencies continuously, predict high-risk inaccuracies, and prioritize remediation efforts.
How AI-Enabled Provider Data Accuracy Works
AI improves provider data quality by evaluating information across multiple sources and over time, rather than relying on point-in-time checks. The following illustration highlights how AI-enabled provider data accuracy can be applied in practice to identify inconsistencies, prioritize risk, and maintain reliable directories as provider networks change.
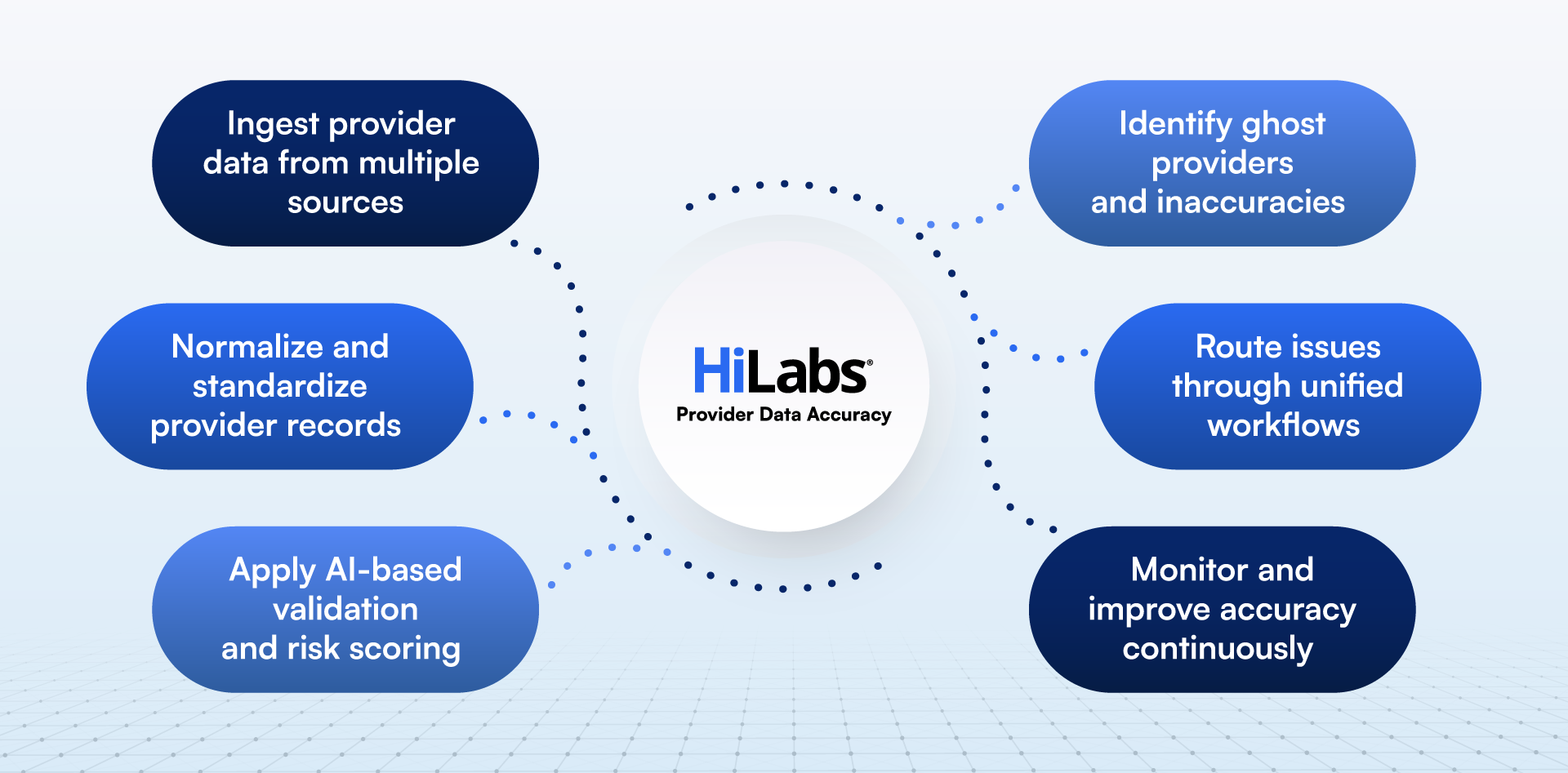
HiLabs offers proprietary, purpose-built AI solutions through its MCheck® suite of applications to enable these capabilities and reduce operational burden for health plans.
How HiLabs Solves Provider Data Management Challenges
HiLabs addresses provider data accuracy through MCheck® Provider Data Accuracy (PDA), an AI-driven solution designed to continuously validate, correct, and enrich healthcare provider data at scale. PDA is built for health plans managing large, complex provider networks where outdated provider contact details, incorrect network status, and retired or inactive providers create compliance risk and member abrasion.
Rather than relying on call campaigns, provider attestations, or self-reported updates as the primary mechanism for directory maintenance, PDA replicates healthcare SME review at scale using HiLabs’ proprietary R3 healthcare LLM.
The model scans thousands of provider data sources—ranging from public and government sources to provider websites and appointment sites—and scores findings for Reliability, Relevance, and Recency (the R3 model) before producing recommended updates.
Continuous Validation at the Cadence Health Plans Need
PDA validates and refreshes provider data on a recurring cadence that aligns to payer operational needs—typically monthly—so directories do not depend on periodic one-time cleanups. This improves ongoing audit readiness and reduces the likelihood that plans can address directory issues before member complaints or regulatory scrutiny.
Where clients require faster turnaround for smaller updates, PDA can also process ad hoc files (for example, ~50,000 provider data records) outside the standard cadence.
Accuracy and Completeness Across 60+ Provider Attributes
Provider directory accuracy is not only about “address correctness.” PDA validates and enriches 60+ provider attributes—such as phone numbers, specialties, and accepting-new-patients signals—by cross-checking signals across thousands of sources. This improves the completeness of member-facing directories while strengthening the defensibility of provider network reporting.
Audit Readiness and No Surprises Act Accountability
Provider directory requirements under the No Surprises Act shift financial risk to health plans when members rely on inaccurate directory information. PDA supports audit readiness by continuously validating network status and ensuring plans can update directories promptly when changes are received—reducing compliance exposure and downstream cost.
Why MCheck® Provider Data Accuracy is Different from Traditional Approaches
Traditional directory maintenance often relies on static databases, periodic audits, and manual verification workflows. PDA differs by applying AI-driven validation across thousands of sources and producing scored recommendations that can be integrated into payer systems with limited-to-no manual intervention.
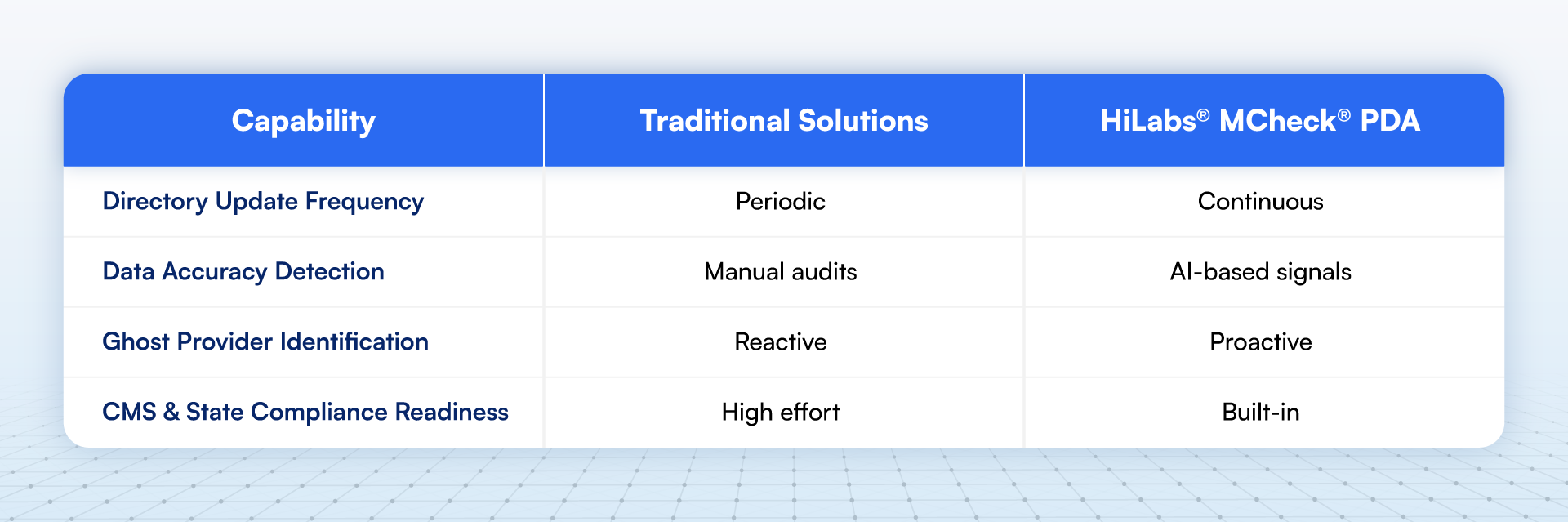
Instead of treating verification as a periodic event, PDA operationalizes continuous directory accuracy—helping plans move from “audit response mode” to sustained accuracy management. For innovative health payers, this shift from traditional to AI-driven provider data management is critical with increasing regulatory scrutiny.
Real-World Impact of Improved Provider Data Accuracy
When provider data accuracy improves, health plans see measurable impact across compliance, operations, and member experience. HiLabs has corrected 100M+ directory errors for 10+ national and regional health plans and maintains 95%+ provider directory accuracy for these customers.
In practice, this translates into fewer member-facing issues caused by outdated or incorrect directory information. Plans also reduce the operational drag of repeated verification cycles, since corrections are informed by validated signals and can be applied more consistently across downstream systems. Over time, improved accuracy supports stronger audit readiness and more defensible directory integrity as regulatory scrutiny increases.

Why Provider Data Management Matters Now
With increasing enforcement of CMS directory accuracy requirements, rising consumer expectations, and expanding networks, health plans can no longer rely on static provider data models.
Accurate, AI-driven, provider data management is now essential for both maintaining compliance and ensuring timely access to care. Adopting advanced, integrated workflows also helps reduce operational costs while protecting brand trust and supporting overall growth. As networks change more frequently, the operational requirement is not just to “fix” directories periodically, but to sustain accuracy on an ongoing cadence.
How HiLabs Integrates With Your Existing Ecosystem
HiLabs integrates seamlessly with:
- Credentialing systems
- Claims platforms
- Provider directories
- Network management tools
This allows health plans to enhance provider data accuracy without disrupting existing operations, making adoption faster and impact measurable.
Because updates are derived from validated signals and delivered in a structured way, plans can operationalize corrections across workflows while reducing manual verification burden and improving the consistency of provider data across the enterprise.
Conclusion
Provider data management is no longer a back-office function; it’s a strategic capability that underpins compliance, network adequacy, and member trust. By improving provider data accuracy, reducing ghost provider exposure, and maintaining compliant directories, health plans can lower regulatory risk. For providers, this reduces the burden of everyday operational workflows. For members, this means improved access to care.
HiLabs transforms payer operations through AI-driven intelligence that cleans provider data and scales with complexity.
Explore how HiLabs improves provider data accuracy and network performance. Learn More →